Mark Dusseau
Aug 6, 2024
Upgrading healthcare infrastructure isn’t just about adding the latest tech—it’s about transforming the way healthcare facilities work to make things more efficient and improve patient care. As healthcare evolves, finding and addressing hidden costs is key to keeping finances in check. In this guide, we’ll break down why modernizing infrastructure is essential, how tech like IoT, AI, and telemedicine is reshaping the field, and practical ways to cut costs. By leveraging data analytics and investing in smart training, healthcare organizations can make the shift smoother and more sustainable. Here’s how these changes can move your practice forward.
Key Points
Updating healthcare infrastructure boosts efficiency, controls hidden costs, and elevates patient care.
Key investments in IoT, AI, and telemedicine are central to building a future-ready healthcare system.
Recognizing and managing hidden costs can make a big difference in budgeting and resource allocation.
Data analytics help fine-tune operations and outcomes, driving down costs while improving care.
Training staff and leading thoughtful change management make a major impact on successful modernization.
Understanding Healthcare Infrastructure
To appreciate why infrastructure matters, it helps to know what it actually covers: the facilities, equipment, tech, and people working together to deliver healthcare. Right now, a lot of systems are dealing with legacy IT that can slow things down and limit growth.
Hospitals and clinics consume a huge chunk of healthcare resources, and infrastructure is a big reason for this. With healthcare demands rising, the ability for different systems to work together smoothly—interoperability—has become crucial. When data flows seamlessly across systems, it enhances patient care and eliminates redundant work.
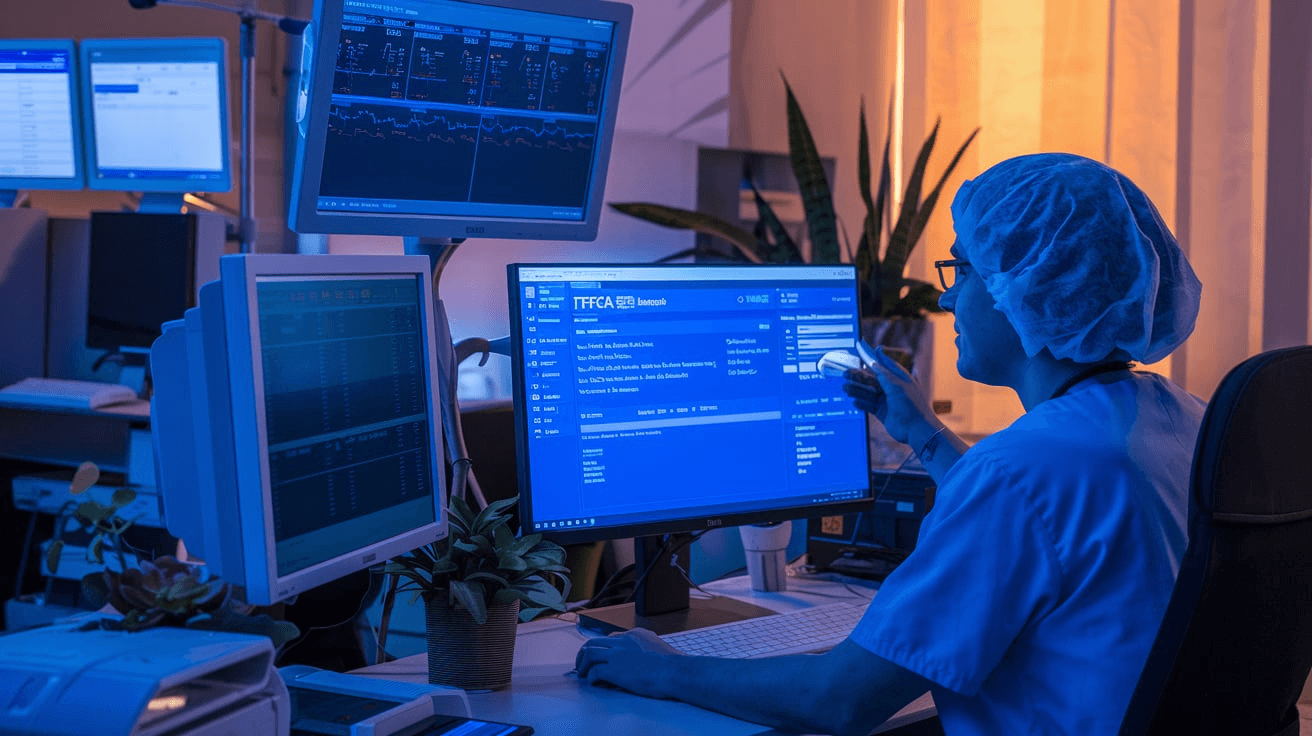
For instance, a fully modern hospital might integrate electronic health records (EHRs), advanced diagnostic tools, and patient monitoring systems, creating a real-time, connected environment for care. This setup means doctors, nurses, and support teams get the info they need right when they need it, improving diagnosis and treatment times.
So infrastructure isn’t just physical—it’s a network that has to be adaptive, resilient, and cost-efficient. We’re talking modular designs that can scale or pivot during crises without draining resources.
The Case for Modernization
Modernizing healthcare isn’t optional anymore. With rising patient expectations and tech advances, healthcare systems have to keep pace to stay competitive and serve their communities effectively.
In today’s digital world, patients expect instant access to records, easy booking, and quick responses from providers. Older IT systems often can’t meet these demands, which can hurt patient satisfaction and push people to other providers.
Interoperability is another huge driver. With so many providers involved in a single patient’s care, easy access to shared data is a must for avoiding errors and redundant tests, and for delivering quality care.
Then there’s security. The stakes are high when it comes to safeguarding sensitive patient data, and healthcare providers need to protect against the growing threat of cyberattacks. Updated systems with strong cybersecurity don’t just secure data; they also help build patient trust.
Financially, outdated systems are a drain. Hidden costs and inefficiencies can eat up resources. Modernizing helps facilities operate more smoothly, cuts unnecessary costs, and lets teams focus on delivering better outcomes.
Key Tech for Healthcare Modernization
To bring healthcare up to speed, adopting key technologies is non-negotiable. Internet of Things (IoT) technology is changing the game by improving real-time patient monitoring and making it easier to share data across the care team. Healthcare IoT means less lag time in decision-making, which lightens the load on the entire system.
Artificial Intelligence (AI) is another major player, helping providers analyze data faster, create personalized treatment plans, and improve resource allocation. With AI, teams get insights that lead to better patient outcomes and more efficient hospital operations.
Telemedicine is another big win, especially when physical access is limited. It keeps patients connected with their providers remotely, extending healthcare’s reach while reducing costs tied to in-person visits.
Together, these tools drive efficiency, make care more accessible, and keep healthcare providers competitive. Embracing them isn’t just a tech upgrade; it’s a foundation for a more connected, efficient, and patient-centered healthcare experience.
Identifying Hidden Costs in Healthcare

Spotting hidden costs is a crucial part of keeping healthcare budgets lean and operations smooth. These costs usually hide out in outdated systems or inefficient processes, quietly draining funds.
A big one? Legacy tech. Maintaining and using old IT systems is a major financial drain. Relying on paper records, for instance, isn’t just inefficient; it’s costly to store and maintain, plus it’s a risk for errors.
Many facilities also have tons of data they’re not fully using. If analyzed properly, this data could reveal inefficiencies like redundant procedures or poor resource allocation. But without data analytics, those insights—and the savings they bring—are lost.
There’s also regulatory compliance. Staying compliant with laws like HIPAA means regular updates to systems, which can be pricey if unplanned. Then there are staffing inefficiencies. Using outdated scheduling systems can lead to overstaffing or understaffing, both of which lead to financial waste or hurt patient care.
By conducting regular audits, healthcare providers can uncover these hidden costs. Moving to the cloud, adopting analytics, and fine-tuning workflows can help facilities stay lean while improving service.
Strategies for Cutting Hidden Costs
Modernizing healthcare infrastructure isn’t just about new tech—it’s about managing the hidden costs that keep adding up. Here are some strategies to find and reduce these costs:
Tech Optimization: It’s not enough to have tech; it needs to be fully utilized. Regular audits help identify underused equipment or software, so you’re not paying for more than you use.
Streamline Admin Processes: Admin inefficiencies add up fast. Automating workflows and integrating EHRs with other systems cuts down on double data entry and improves efficiency.
Inventory Management: Proper supply chain management keeps stock levels in check and reduces waste. Just-in-time inventory can help avoid overstocking or shortfalls.
Energy Efficiency: Upgrades like LED lighting, better insulation, and energy management systems cut down on utility costs.
Value-Based Care Models: Moving from fee-for-service to value-based care can reduce costs while focusing on patient outcomes rather than volume.
By focusing on these areas, healthcare providers can reduce hidden costs and improve overall efficiency.
The Role of Data Analytics in Cutting Costs
Data analytics is a powerful tool for saving on healthcare costs. Here’s how it makes a difference:
Better Resource Management: Analytics helps predict demand, so hospitals and clinics can staff and allocate resources more accurately.
Reducing Readmissions: With data analytics, providers can identify the factors that lead to patient readmissions, reducing costs and improving care.
Supply Chain Optimization: Data-driven insights streamline restocking, so facilities avoid both shortages and overstock.
Fraud Detection: Analytics helps detect billing anomalies early, protecting against costly fraud.
Enhanced Decision-Making: With precise patient data insights, clinicians can improve diagnoses and treatments, saving costs on ineffective approaches.
Data analytics doesn’t just boost operational efficiency—it keeps healthcare institutions on a sustainable cost track.
Investing in Training and Change Management
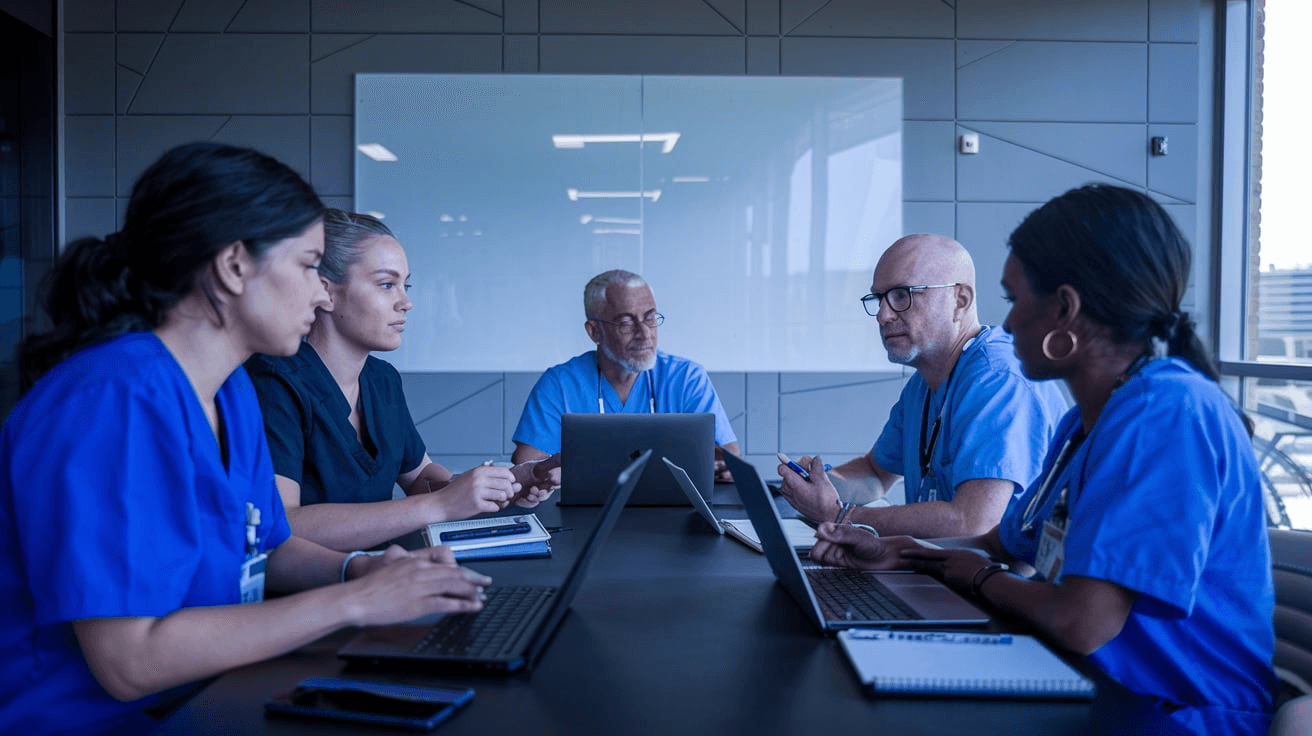
Rolling out new systems means investing in staff training and change management. This part is crucial because a well-trained workforce can fully leverage new tech to improve patient care and streamline operations.
Effective training fills in skill gaps, cuts down on errors, and reduces resistance to change. Change management, meanwhile, helps create an environment that welcomes transformation. It’s about involving the whole team in the journey from the start and making sure everyone understands why these changes matter.
For a smooth transition, everyone—from frontline workers to leadership—needs the skills to work with the new systems and navigate both old and new tech. This human investment makes sure your healthcare facility doesn’t just modernize but keeps improving in the long run.
What’s Next for Healthcare Infrastructure?
As healthcare infrastructure moves forward, expect big changes. Blockchain technology, for example, will improve data security and patient privacy while reducing redundant admin tasks.
Telehealth is here to stay, especially as demand for remote healthcare services grows, and smart hospitals equipped with IoT devices are on the rise, offering predictive maintenance to keep vital equipment running smoothly.
In the future, AI-driven healthcare planning will drive efficiency by helping healthcare providers anticipate patient needs and allocate resources more precisely. And as the industry focuses more on sustainability, we’ll see healthcare infrastructure adopt more eco-friendly practices, from energy-efficient buildings to smarter resource management.
For healthcare institutions looking to modernize while cutting hidden costs, schedule a consultation to discuss tailored strategies. Staying competitive and delivering high-quality care through efficient, modern infrastructure will be key.
Wrapping Up
Modernizing healthcare infrastructure is critical for cutting hidden costs and improving patient care. Technologies like AI and IoT bring serious advantages—not just in terms of operations but in real patient outcomes. Embracing these changes prepares healthcare providers for future challenges. Investing in modernization and data analytics is the way forward for a more efficient, cost-effective healthcare environment. Keep pushing the needle on innovation and stay at the forefront of healthcare.